IEMIG nel 2023 ripresenta il PREMIO VALENTINA LIBONI – il premio sarà riservato alle migliori tesi di laurea in medicina, specializzazione in medicina di urgenza e laurea in scienze infermieristiche,
IEMIG nel 2023 ripresenta il PREMIO VALENTINA LIBONI – il premio sarà riservato alle migliori tesi di laurea in medicina, specializzazione in medicina di urgenza e laurea in scienze infermieristiche,
SOCCORRAMI: difendiamo la città dalle emergenze Festa della Mamma 13 maggio 2023 9.30-13.00 IEMIG continua a veleggiare nel campo della informazioni e diffusione della cultura di emergenza – Prossimamente IEMIG
La Drssa Bagatti, anestesista rianimatore , ci conduce per mano all’interno del mondeo della DONAZIONE . LA donazione degli organi negli ultimi annoìi ha assunto un ruolo strategico nel processo
A 57 year-old-patient is brought in Emergency Department by ambulance complaining of fever, swelling and erythema of the left leg .Medical History: not relevant.Vital Signs: BP 130/80 mmHg, HR 90
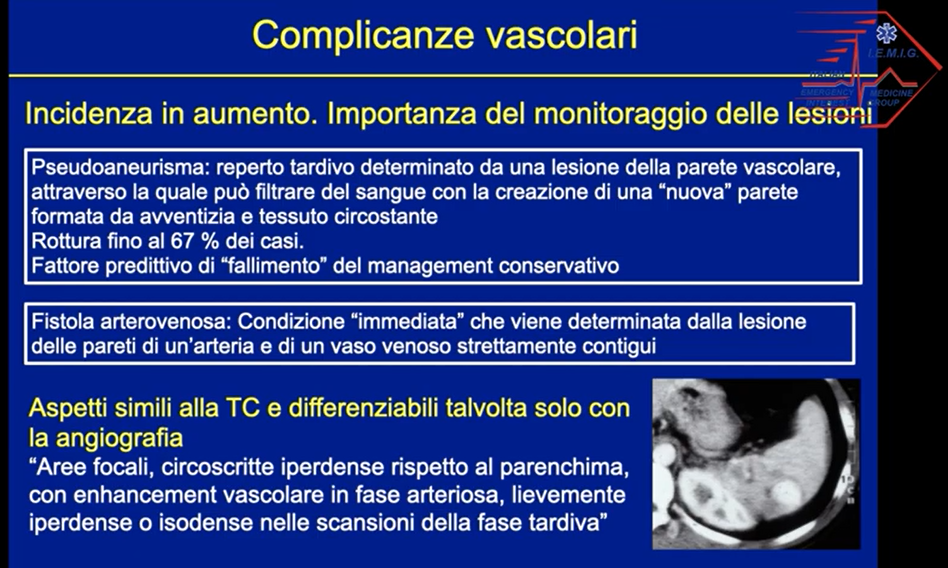
Una lezione sui traumi addominali chiusi a cura della Dott.ssa Stefania Salti e Dott. Andrea Bulli – UO Radiologia, Nuovo Ospedale di Prato Santo Stefano.
