IEMIG nel 2023 ripresenta il PREMIO VALENTINA LIBONI – il premio sarà riservato alle migliori tesi di laurea in medicina, specializzazione in medicina di urgenza e laurea in scienze infermieristiche,
IEMIG nel 2023 ripresenta il PREMIO VALENTINA LIBONI – il premio sarà riservato alle migliori tesi di laurea in medicina, specializzazione in medicina di urgenza e laurea in scienze infermieristiche,
La Drssa Bagatti, anestesista rianimatore , ci conduce per mano all’interno del mondeo della DONAZIONE . LA donazione degli organi negli ultimi annoìi ha assunto un ruolo strategico nel processo
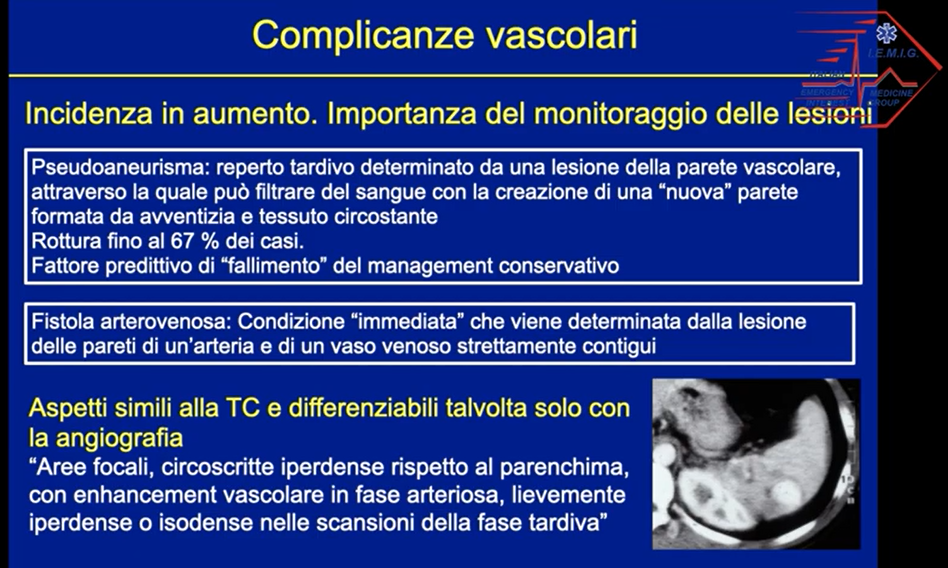
Una lezione sui traumi addominali chiusi a cura della Dott.ssa Stefania Salti e Dott. Andrea Bulli – UO Radiologia, Nuovo Ospedale di Prato Santo Stefano.
A cura della Dott.ssa Sara Bagatti, Coordinatrice locale alla donazione di organie tessuti del Nuovo Ospedale Santo Stefano di Prato e dell’Azienda Ospedaliero Universitaria Careggi, nonchè coordinatrice dell’Area Vasta Toscana
Grazie ad AMI ( associazione ONLUS Materno Infantile . Ospedale Santo Stefano – PRATO) – IEMIG ha partecipato alla Giornata della FESTA DELLA MAMMA” , manifestazione tenutasi nei nuovi giardini
